Migraine disease transcends the realm of ordinary headaches, symbolizing a complex neurological challenge that can deeply affect one’s daily life. To understand migraine disease better, it’s crucial to explore the intricate relationship between the trigeminocervical complex (TCC), the trigeminal and occipital nerves, and how they contribute to migraine pain. This post aims to demystify this connection, providing insights into the mechanisms behind migraine and potential avenues for relief.
The Trigeminocervical Complex: The Brain’s Pain Processing Center
The Trigeminocervical Complex (TCC) is a critical structure within the brainstem that serves as a hub for processing pain and sensory information from the head and neck. This is where the trigeminal nerve, which is responsible for sensations in the face, head, and parts of the neck, converges with the upper cervical spinal nerves.
The convergence of the trigeminal and occipital nerves at the TCC is a key aspect of its function. The trigeminal nerve, with its three major branches (ophthalmic, maxillary, and mandibular), carries sensory information from the face, scalp, and meninges. Meanwhile, the occipital nerves, arising from the upper cervical spinal roots, transmit sensations from the back of the head.
When these nerves converge at the TCC, they create a network that allows for the integration of sensory inputs from a wide area of the head and neck.
The Role of TCC in Migraine
At the heart of migraine pain lies the trigeminocervical complex, a region in the brainstem that plays a pivotal role in processing pain signals from the head and neck. The TCC integrates sensory information, particularly pain, from the face, head, and cervical region. This integration is crucial for understanding the intensity and location of pain, making the TCC a key player in the migraine puzzle.

Figure 1. Diagram of Trigeminocervical Complex (TCC)
The Trigeminal Nerve: The Messenger of Pain
The trigeminal nerve, the largest cranial nerve, acts as the primary messenger of pain and sensory information from the head and face to the brain. It has three major branches: the ophthalmic, maxillary, and mandibular, which cover a broad area from the scalp to the jaw. When it comes to migraine, the trigeminal nerve’s role is significant. It can become hyperactive and send excessive pain signals to the brain, leading to the throbbing, pulsating pain characteristic of migraine.
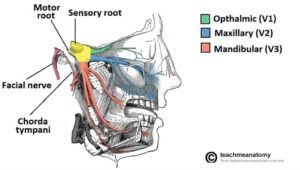
Figure 2. Diagram of Trigeminal Nerve; https://techmeanatomy.info
The Occipital Nerves: Linking the Neck and Head
The occipital nerves, including the greater, lesser, and third occipital nerves, are primarily responsible for transmitting sensations from the back of the head to the top. While less discussed in the context of migraine, these nerves can also contribute to migraine pain, especially in cases where the pain extends from the neck to the head. This connection highlights the importance of considering the entire head-neck region in migraine management.
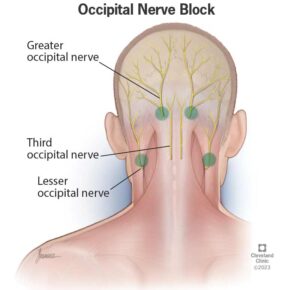
Figure 3. Diagram of Occipital Nerve; https://my.clevelandclinic.org
The Connection: How It All Ties Together
The relationship between the TCC, the trigeminal nerve, and the occipital nerves is complex and interwoven. During a migraine attack, a cascade of neurological events is triggered, starting with the activation of the trigeminal nerve. This activation leads to the release of inflammatory substances around the brain’s blood vessels and the TCC, amplifying pain signals.
Simultaneously, the occipital nerves can become involved, especially if the migraine pain spreads to the back of the head. This involvement creates a feedback loop, where pain signals from the occipital region further stimulate the TCC, intensifying the migraine experience.
Breaking the Cycle: Approaches to Migraine Management
Understanding the roles of the TCC, trigeminal, and occipital nerves in migraine pain opens up new avenues for treatment. Traditional approaches like medications aim to block pain signals or reduce inflammation. However, advancements in neuromodulation therapies offer promising alternatives.
Neuromodulation techniques, such as transcranial magnetic stimulation (TMS), occipital nerve stimulation (ONS), and Combined Occipital Trigeminal Neurostimulation (COT-NS) target these neural pathways directly. By modulating the activity of the trigeminal and occipital nerves and influencing the TCC, these therapies can disrupt the pain signal cascade, offering relief to many sufferers.
Lifestyle and Preventive Measures
Beyond medical interventions, understanding the neural underpinnings of migraine can empower individuals to adopt lifestyle changes that may mitigate the frequency and severity of attacks. Stress management, regular exercise, and avoiding known triggers can help maintain a balance in the nervous system, potentially reducing the hyperactivity of the trigeminal and occipital nerves.
The Future of Migraine Research
The exploration of the relationship between the TCC, trigeminal, and occipital nerves is an ongoing journey. As research delves deeper into these connections, the hope is to uncover more precise and effective treatments that can provide relief without the side effects often associated with current therapies.

Relivion MG: A Harmonious Solution
In the quest for effective migraine management, Relivion MG emerges as a particularly promising therapy, thanks to its unique interaction with the brain’s intricate pain processing network. This device stands out because it directly engages with the key players in migraine pain: the trigeminocervical complex, the trigeminal nerve, and the occipital nerves. The added benefit is that this is an external stimulation, so it does not require complex surgeries like implantable devices.
Here’s why Relivion MG is an ideal therapy for those seeking relief from the relentless grip of migraine:
- Targeted Neuromodulation
Relivion MG employs advanced neuromodulation technology to deliver focused stimulation to the trigeminal and occipital nerves. This precise approach ensures that the therapeutic effects are concentrated exactly where they’re needed, modulating the pain signals at their source. By directly influencing these nerves, Relivion MG can disrupt the pain signal cascade that leads to migraine symptoms, offering relief to those living with Migraine disease.
- Engaging the Trigeminocervical Complex
The device’s innovative design allows for the simultaneous stimulation of multiple nerve branches, ensuring that the TCC—the brain’s central hub for pain processing—is effectively modulated. This comprehensive engagement with the TCC can help to dampen the hyperactivity that contributes to migraine pain, providing a soothing effect that addresses the root cause of migraine.
- Non-Invasive and Drug-Free
One of the most appealing aspects of Relivion MG is its non-invasive nature. Unlike some treatments that require medication or invasive procedures, Relivion MG offers a drug-free alternative that minimizes the risk of side effects. This makes it an ideal option for those who are looking for a safe and gentle approach to migraine management.
- Personalized Therapy
Recognizing that each individual’s experience with migraine is unique, Relivion MG is designed to offer personalized therapy. Users can adjust the intensity and duration of the stimulation, tailoring the treatment to their specific needs and ensuring the most effective relief possible.
The introduction of Relivion MG into the landscape of migraine therapies represents a significant advancement in our ability to manage this complex condition. By harmonizing with the body’s natural neural pathways and offering a targeted, non-invasive solution, Relivion MG is at the forefront of a new era in migraine care. As we continue to explore the potential of neuromodulation in addressing neurological conditions, Relivion MG stands as a testament to the power of innovative, patient-centered therapy.

Conclusion
Migraine disease is a multifaceted condition with deep neurological roots. The interplay between the trigeminocervical complex, and the trigeminal and occipital nerves, is central to understanding and managing migraine pain. By continuing to explore these connections, the medical community moves closer to unraveling the mysteries of migraine, offering hope to millions of sufferers worldwide. As we advance, the promise of new treatments and a deeper understanding of migraine lies on the horizon, bringing us closer to a world where migraine pain can be effectively managed or even prevented.
The intricate dance between the trigeminocervical complex, the trigeminal and occipital nerves, and migraine pain requires a nuanced approach to therapy. Relivion MG, with its precise neuromodulation and personalized treatment options, offers a beacon of hope for those navigating the turbulent waters of migraine management. Its alignment with the brain’s natural pain-processing mechanisms makes it an ideal choice for those seeking a harmonious path to relief.
References:
- Akerman S, Romero-Reyes. Insights Into the Pharmacological Targeting of the Trigeminocervical Complex in the Context of Treatments of Migraine 2013;13(9):1041-1059
- Bartsch T, Goadsby PJ. The trigeminocervical complex and migraine: current concepts and synthesis. Curr Pain Headache Rep. 2003 Oct;7(5):371-6. doi: 10.1007/s11916-003-0036-y. PMID: 12946290.
- Burstein, R., Noseda, R., & Borsook, D. (2015). Migraine: multiple processes, complex pathophysiology. Journal of Neuroscience, 35(17), 6619-6629.
- Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of Migraine: A Disorder of Sensory Processing. Physiological Reviews, 97(2), 553-622.
- May, A. (2019). Understanding migraine as a cycling brain syndrome: reviewing the evidence from functional imaging. Neurological Sciences, 38(Suppl 1), 125-130.
- Ashina, M., Bendtsen, L., Lyngberg, A. C., Lipton, R. B., Hajiyeva, N., & Jensen, R. (2015). Prevalence of neck pain in migraine and tension-type headache: A population study. Cephalalgia, 35(3), 211-219.
- Andreou, A. P., & Edvinsson, L. (2019). Mechanisms of migraine as a chronic evolutive condition. Journal of Headache and Pain, 20(1), 117.
- Dodick, D. W. (2018). A Phase-by-Phase Review of Migraine Pathophysiology. Headache: The Journal of Head and Face Pain, 58(Suppl 1), 4-16.

